Abstract
Introduction: Sickle Cell Disease (SCD) is the most common inherited blood disorder, affecting over 100,000 people in the United States. The latest medical managements have yielded better outcomes in mortality and morbidity among people with SCD. Despite these advancements, emerging young adults have complications transitioning from pediatric care to adult care and remain with the highest mortality rate in the population. Got Transition is a federally funded national resource center that aims to support youth and young adults moving from pediatric to adult care by implementing the Six Core Elements of Transition. At our institution, we established a transition program aimed at improving clinical care, medical management, and improvement in the transition from pediatric to adult medical care. Our goal was to develop a standardized, age appropriate sickle cell education curriculum to implement at clinic visits for our patients aged 13 and older.
Hypothesis: We hypothesize that with a structured transition curriculum, we would be able to improve patient knowledge in medical aspect of the disease, academic resources and a better understanding of their complex psychosocial needs.
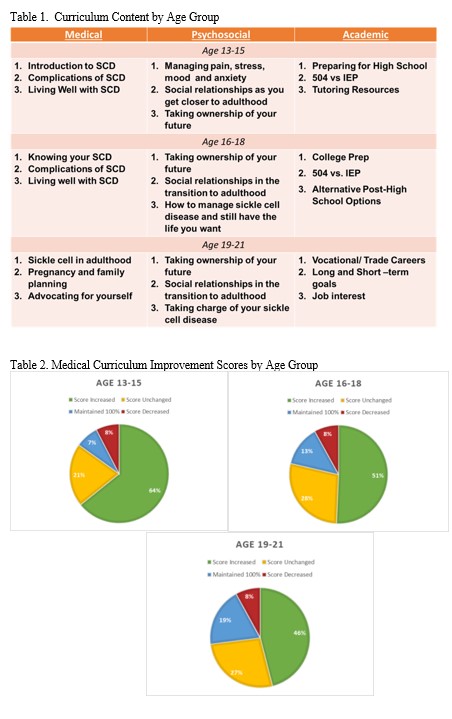
Methods: We developed a transition program called Adolescent and Young Adult Sickle Cell Uplift and Learn Program for Transition (AYA SCULPT) that would focus on patients starting at 13 years old with a multidisciplinary approach of care. We adopted the Got Transition model implementing the Six Core Elements of Transition. Our team not only wanted to address educational topics related to their medical care, but also psychosocial and academic topics. A transition education curriculum was created spanning three age groups on the three major topics and further broken up into three smaller sections for clinic use to accommodate for time restraints (Table 1). A pilot of the medical curriculum was started August 2019 addressing medical topics relating to better understanding of sickle cell disease. We then introduced our psychosocial curriculum in January 2021. A member of our comprehensive sickle cell team provides the four-question pre-test to the patient at the beginning of their regularly scheduled clinic appointment. At the end of the appointment the nurse or provider will grade the pre-test and provide verbal education as well as printed material on the topics for the day. Scoring and topics are tracked in the patient's note as well as in a transition education database. At the patient's next visit, the same test is administered as a post-test in order to determine knowledge acquired and retention of the materials. Post-test scores are also recorded in the patient note and transition education database. Once the patient finishes a module, we move to the next topic at the next regularly scheduled visit. Depending on the patient's genotype and medication management, post-tests can be given between two to six months after the pre-test.
Results: Scores from pre-test were compared to those of post-test for patients that had the opportunity to complete the medical curriculum quizzes. One hundred and fifty six patients range from age 13-21 were included in this pilot study. Of patients aged 19-21, 69% have taken at least one pre-test and post-test for the medical education (63 total pre- and post-tests). Forty-three (78%) patients aged 16-18 have taken at least one pre-test and post-test (75 total pre- and post-tests). Thirty-three (67%) patients aged 13-15 have taken at least one pre-test and post-test (53 total pre- and post-tests). Results were categorized as score increased, score unchanged (pre-test score was not 100%), maintained 100% (unable to increase in score), and score decreased. In every age group, the category with the most results was "score increased." Shown in Table 2.
Conclusion: Further extrapolation suggests that the medical curriculum provided in clinic improves the sickle cell knowledge in this adolescent and young adult population. Though all age groups improved, the biggest improvement was noted in knowledge with our 13-15 year olds. These results suggest that early transition education can be impactful even if started at the early phases of adolescence. Studies are still ongoing with our medical curriculum and early psychosocial data is beginning to support our previous findings. As part of transition health care, focusing on disease education can provide better knowledge and hopefully improve patient outcomes.
Clay: Novartis: Honoraria; GBT: Membership on an entity's Board of Directors or advisory committees.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal